When it comes to understanding medical bills, the details matter. Getting things right means the difference between smooth payments and financial nuisances.
The three essential codes help to make things clear: modifiers 59, 25, and 91. They act like translators, ensuring physician services are clear to insurance companies. By doing this, they confirm they understand everything and that the physicians get paid correctly.
These modifiers can help to ensure that medical bills are accurate and that physicians are paid correctly.
But why do these specific modifiers matter so much? And how do they function in the medical bill submission? Before this, you need to understand what modifiers in medical billing are.
Modifiers in medical coding are like precision and transparency tools. They add essential details to the main codes describing a physician’s services, ensuring that the precise nature of the treatment is captured. By using modifiers, healthcare providers can better depict a patient’s visit, ensuring they receive the proper reimbursement for their services.
Modifier 59
Modifier 59 is more than just an add-on code. It’s a way to signal that a physician provided multiple services in one session, but they are distinct and independent of each other. It indicates that the services are not overlapping but necessary in their own right.
How does it work?
When billing for medical services, primary procedure codes define the main services. If additional procedures or services aren’t typically paired with the primary service, Modifier 59 is appended to the other service’s code. That tells the insurance company that the service is not part of the primary service.
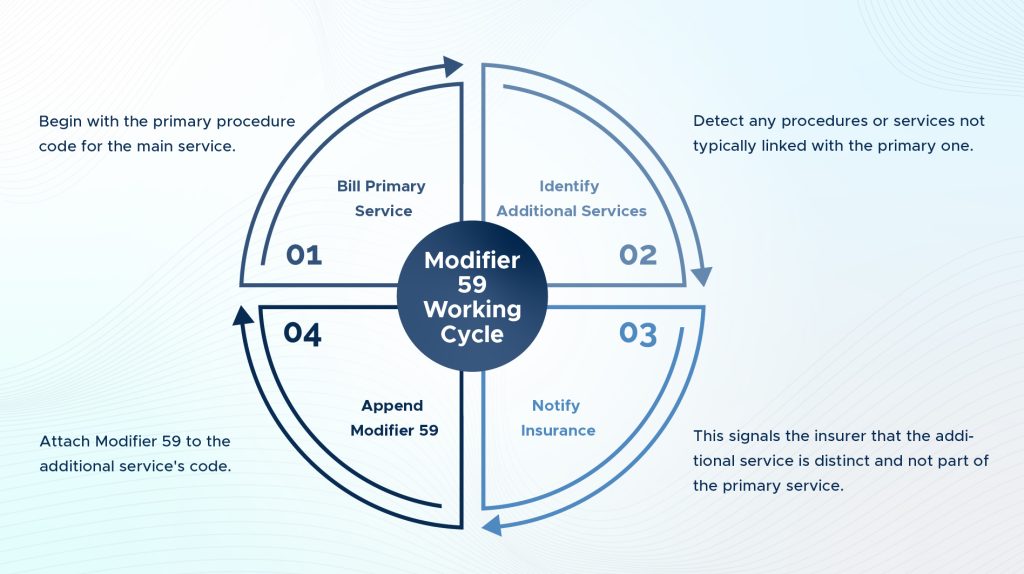
Working cycle
Here’s a concise working cycle for using Modifier 59 in medical billing:
Bill Primary Service. Begin with the primary procedure code for the main service.
Identify Additional Services. Detect any procedures or services not typically linked with the primary one.
Append Modifier 59. Attach Modifier 59 to the additional service’s code.
Notify Insurance. This signals the insurer that the additional service is distinct and not part of the primary service.
When to use
- When the same physician or other qualified healthcare professional performs a procedure or service subsequent to a related procedure or service on the same day.
- When the subsequent procedure or service is unrelated to the first procedure or service but is performed during the same session.
When not to use
- When the subsequent procedure or service is planned and part of the global surgical package for the first procedure or service.
- When a different physician or other qualified healthcare professional performs the subsequent procedure or service.
- When the subsequent procedure or service is performed on a different day than the first procedure or service.
Practical examples
➜ Suppose a patient comes in with a deep cut on the arm and, after addressing the wound, also asks for a separate unrelated mole removal. Both procedures are done in the same session. Modifier 59 would indicate that the mole removal was an independent service.
➜ A patient visits an orthopedic surgeon for knee and shoulder pain. The physician vaccinates injections in both areas during the same visit. Though injections are given in one session, each is a separate service. Modifier 59 can be attached to the additional procedure code to highlight its distinct nature.
Common mistakes and misconceptions
One of the frequent misconceptions is that Modifier 59 is a “universal” modifier that can be added whenever there’s more than one service. This isn’t true; its specific use is for distinct procedural services.
Another mistake is using Modifier 59 for services that are typically bundled together. For example, if a patient gets a consultation during a single visit and then a standard follow-up procedure is typically done post-consultation, Modifier 59 wouldn’t be appropriate.